Introduction:
Amalgatome® MD study outcome in graft recovery and skin yield.
 Donated cadaveric skin, also known as allograft skin or, in the past, homografts, has an important place in wound care. Traditionally, this biological material was primarily, and probably only, used in burn care, where it still has a major role as a dressing for partial thickness burns1 temporary coverage prior to autografting in excised full thickness burns2 and as an overlay in the sandwich and intermingled techniques where a (widely meshed) autograft is protected from desiccation and mechanical damage by a narrowly meshed allograft on top3. Cadaver skin also has found a place in the management of venous leg ulcers and diabetic foot ulcers4, 5 and it also has become the source material for a series of biologically based matrices6, 7.
Donated cadaveric skin, also known as allograft skin or, in the past, homografts, has an important place in wound care. Traditionally, this biological material was primarily, and probably only, used in burn care, where it still has a major role as a dressing for partial thickness burns1 temporary coverage prior to autografting in excised full thickness burns2 and as an overlay in the sandwich and intermingled techniques where a (widely meshed) autograft is protected from desiccation and mechanical damage by a narrowly meshed allograft on top3. Cadaver skin also has found a place in the management of venous leg ulcers and diabetic foot ulcers4, 5 and it also has become the source material for a series of biologically based matrices6, 7.
Most cadaver skin, whether for local use, for use in a skin bank or for distribution to a commercial institution, is procured by skin recovery services. The dermatomes used for the procurement of cadaver skin are the same type of equipment that is used in the operating room for obtaining autografts from patients. However, in burn care, and particularly in large, full thickness burns, the available donor sites may be limited and, thus, the grafts often have to be taken from anatomically difficult and diverse areas8, 9: they may be narrower and/or shorter than in the ideal situation but, indeed, their availability is limited by the patient.
Cadaveric tissue donors usually have many more and superior (with regard to continuance of undamaged skin areas) donor sites available and a harvesting team will try to get allografts that are as long as possible and consistent in depth and width over the entire length of the graft.
While a lot of literature is available on skin banking and the techniques for preserving cadaver skin10-12, surprisingly little literature (if any) is available on the technique of procuring skin from cadaveric tissue donors. However, a number of practical aspects are usually assumed amongst the tissue recovery teams:
- A single long piece of recovered allograft is better than several shorter ones.
- Getting consistent depth and width along the graft becomes more difficult when the graft increases in length.
- For certain areas, i.e. the inner thighs, strongly curved areas and bony prominences recovery is difficult, due to the design of the most commonly used types of dermatome.
- Dermatomes should be easy to assemble, to take apart and to sterilize.
- It is time consuming to have to change blades a number of times during the procurement of all sites of one donor and a high number of blades per donor increases the overall cost of procurement.
A New Dermatome Design
A new dermatome has been developed for the specific purpose of ameliorating these problems.
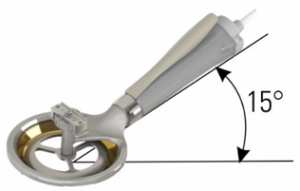 The Amalgatome MD is designed around a blade that rotates instead of making the oscillating movement that a standard dermatome makes. The areas around the blade are contoured: this combination of features enables a dissection range of 180 degrees. The new dermatome has to be pulled instead of being pushed, which, in itself, makes for better control of the movements, better flattening of the area just prior to cutting, and allows the operator to have a direct view on the graft taken (and, when necessary, adjusting the depth setting “in any situation”). The depth gauge plate on the instrument is designed to flatten the skin as it approaches the cutting edge.
The Amalgatome MD is designed around a blade that rotates instead of making the oscillating movement that a standard dermatome makes. The areas around the blade are contoured: this combination of features enables a dissection range of 180 degrees. The new dermatome has to be pulled instead of being pushed, which, in itself, makes for better control of the movements, better flattening of the area just prior to cutting, and allows the operator to have a direct view on the graft taken (and, when necessary, adjusting the depth setting “in any situation”). The depth gauge plate on the instrument is designed to flatten the skin as it approaches the cutting edge.
The handle has a 15% angle versus the blade, minimizing the need for the operator to put pressure on the dermatome, thus reducing inconsistencies in the thickness of the graft. The depth gauge is designed to have a functional range of .000 inches to .045 inches (0.00mm to 1.14mm). The Amalgatome MD cuts to 4 inch (approx. 10 cm) width.
The entire design also aims at better maneuverability which results in longer grafts and grafts can be taken from areas that cannot be used with the “standard” dermatomes, including skin over bony prominences and contoured areas (Figure I).
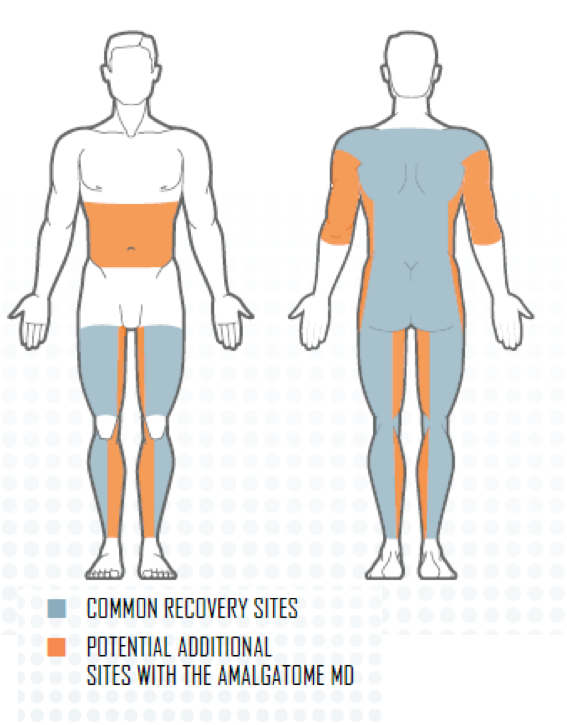
Figure I
The overall goal of the design is to provide a system that allows for faster procurement of the skin with less fatigue and to obtain longer pieces of allograft skin that are more uniform and consistent with regard to their thickness.
These prospective claims were tested using the survey on usage properties.
Survey Methods
Technicians from several skin recovery agencies were asked to participate in a survey on practical aspects of the new dermatome. In the survey a series of questions were asked in regards to different features, specifically:
- Was the dermatome easy to assemble (easy, difficult, or impossible)?
- Was the dermatome easy to operate (very, somewhat, or didn’t use)?
- How would you rate the quality of the skin graft (satisfactory, too think, or too thin)?
- How would you rate the Quick Reference Guide (helpful, didn’t use, or unnecessary)?
- Rate your overall experience with the dermatome (recommend, indifferent, or would not recommend)?
In addition, data from 22 tissue banks from various U.S. locations were obtained on the amount of skin recovered with their traditional, and the new system.
Results
The study was executed from July 2013 to October 2014. 85 personnel from 12 tissue banks participated. On average, the survey participants had 5.1 years of experience (min: 3 months, max. 20 years). Within the survey population the “standard” dermatome was Padgett (60%) or Zimmer (40%). All centers received a total of 20 blades for testing.
Data were collected on 109 donors with 119 separate donor sites. For all donors, the skin was prepped with surgical soap and, for lubrication, mineral oil or 50/50% chlorhexidine with 0.9% saline was used.
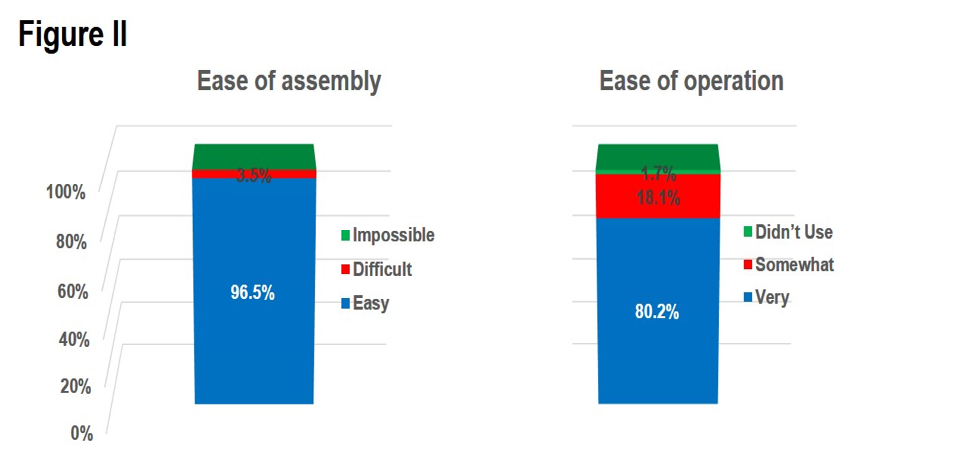 Numbers are expressed as a percentage of the number of donor sites for which a question was answered. For 97% (N=115) of all evaluated donor sites ease of assembly was rated, with 97% (N=111) of these ratings being “easy” and 4% being difficult (Figure I). For 98% (N=116) of all donor sites ease of operation was rated, with an 80% score (N=93) of “very easy”, an 18% score (N=21) of “somewhat easy” and a 2% score (N=2) of “did not use.” (Figure II).
Numbers are expressed as a percentage of the number of donor sites for which a question was answered. For 97% (N=115) of all evaluated donor sites ease of assembly was rated, with 97% (N=111) of these ratings being “easy” and 4% being difficult (Figure I). For 98% (N=116) of all donor sites ease of operation was rated, with an 80% score (N=93) of “very easy”, an 18% score (N=21) of “somewhat easy” and a 2% score (N=2) of “did not use.” (Figure II).
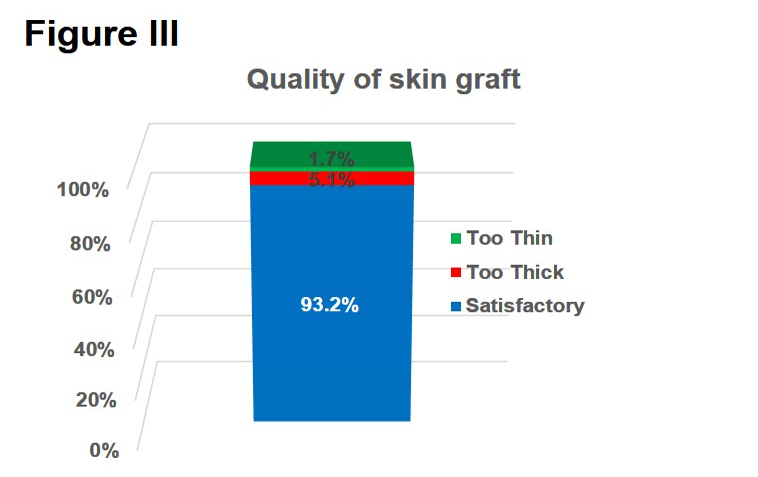 Information on the quality of the obtained skin was provided for 98% for all donor sites (N=117) and was rated satisfactory in 93% (N=109) of all cases. 5 percent of the answers (N=6) stated the skin was too thick and in 2% (N=2) the skin was considered too thin (Figure III).
Information on the quality of the obtained skin was provided for 98% for all donor sites (N=117) and was rated satisfactory in 93% (N=109) of all cases. 5 percent of the answers (N=6) stated the skin was too thick and in 2% (N=2) the skin was considered too thin (Figure III).
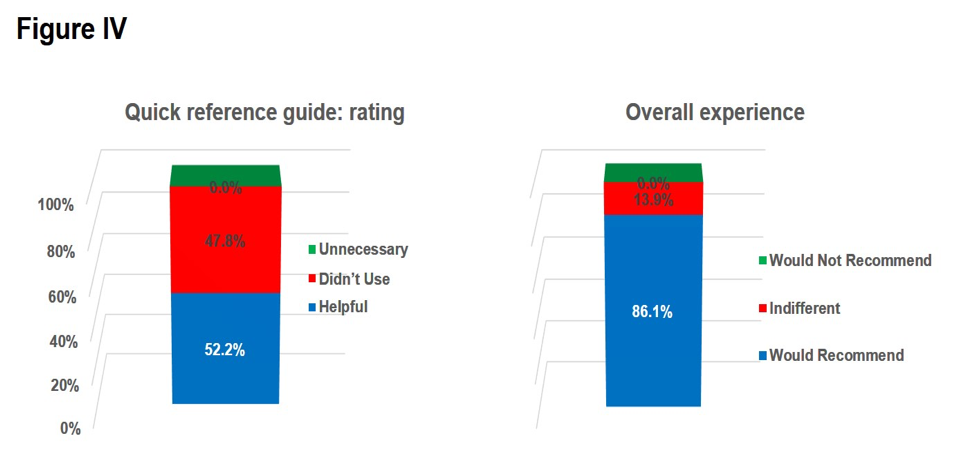
Questions on the Quick Reference Guide were answered for 97% of all donor sites (N=-115): 52.0% (N=60) of participants judged the guide “helpful” and 48% did not use the guide (Figure IV). A question on whether the recovery technician would recommend the new dermatome was answered for 97% of all donor sites (N=115) and 85% (N=99) of these answers was positive while in 14% (N=16) the answer was “indifferent” (Figure III).
On average, only one blade per donor was necessary.
 Recovery data was obtained from 22 tissue banks. On average 2.106 cm2 (2.2 ft2) per donor was recovered with the previously used dermatomes, versus, on average, 3.116 cm2 (3.4 ft2) with the new system. This signifies an increase in skin recovery of 48% per donor.
Recovery data was obtained from 22 tissue banks. On average 2.106 cm2 (2.2 ft2) per donor was recovered with the previously used dermatomes, versus, on average, 3.116 cm2 (3.4 ft2) with the new system. This signifies an increase in skin recovery of 48% per donor.
Discussion and Conclusion
As mentioned, there is limited published information on dermatomes, used in skin recovery available. Thus, a truly scientific comparison of data is not possible. However, given that the average experience of the tissue recovery technicians was 5.1 years, their assumption on practical aspects of skin recovery and dermatome properties are well founded.
Ratings for the different practical aspects of the new dermatome were generally very positive. The fact that 48% of all participants did not use the reference guide may help conclude that the device is very easy to use. The score of 2% for “did not use” on the “ease of use” question may be explained by the fact that many of the surveyed work occurred in teams where one person assembled a device for another one who actually used it.
Ease of usage (assembly and operation) scored very high and the result, with regard to quality of the recovered skin, was satisfactory in 93% of all cases. A higher yield, in combination with a significantly lower percentage of skin that had to be discarded indicates an improved quality system. The survey participants estimated that, with their previous dermatomes, an average of 4.5 blades were used per donor while, with the Amalgatome MD, they needed only one blade. This reduction in the number of blades, plus the combination of a higher yield and decrease in the amount of skin to be discarded during processing contributes to a substantial increase in usable skin and, probably, a significant reduction in operational costs.
In summary, the Amalgatome MD dermatome allowed for an increase in the amount of usable skin per donor while, at the same time, offering a high level of positive aspects related to its usage.
References
- Hermans MH. Clinical experience with glycerol-preserved donor skin treatment in partial thickness burns. Burns Incl Therm Inj 1989;15(1):57-9.
- Hussmann J, Russell RC, Kucan JO, Hebebrand D, Bradley T, Steinau HU. Use of glycerolized human allografts as temporary (and permanent) cover in adults and children. Burns 1994;20 Suppl 1:S61-5; discussion S65-6.
- Kreis RW, Mackie DP, Hermans RR, Vloemans AR. Expansion techniques for skin grafts: comparison between mesh and Meek island (sandwich-) grafts. Burns 1994;20 Suppl 1:S39-42.
- Landsman AS, Cook J, Cook E, Landsman AR, Garrett P, Yoon J, et al. A retrospective clinical study of 188 consecutive patients to examine the effectiveness of a biologically active cryopreserved human skin allograft (TheraSkin(R)) on the treatment of diabetic foot ulcers and venous leg ulcers. Foot Ankle Spec 2011;4(1):29-41.
- Tice DA, Zerbino V. Clinical experience with preserved human allografts for vascular reconstruction. Surgery 1972;72(2):260-7.
- Juhasz I, Kiss B, Lukacs L, Erdei I, Peter Z, Remenyik E. Long-term followup of dermal substitution with acellular dermal implant in burns and postburn scar corrections. Dermatol Res Pract 2010;2010:210150.
- Cheng A, Saint-Cyr M. Comparison of different ADM materials in breast surgery. Clin Plast Surg 2012;39(2):167-75.
- Belczyk R, Stapleton JJ, Blume PA, Zgonis T. Plantar foot donor site as a harvest of a split-thickness skin graft. Clin Podiatr Med Surg 2009;26(3):493-7, Table of Conntents.
- Khalid K, Tarar MN, Mahmood F, Malik FS, Mehrose MY, Ata ul H. Scalp as a donor site for split thickness skin grafts. J Ayub Med Coll Abbottabad 2008;20(1):66-9.
- Dvorankova B, Broz L, Pafcuga I, Kapounkova Z, Konigova R. The role of skin bank in the treatment of severely burnt patients. Acta Chir Plast 2004;46(2):51-5.
- Gaucher S, Khaznadar Z, Gourevitch JC, Jarraya M. Skin donors and human skin allografts: evaluation of an 11-year practice and discard in a referral tissue bank. Cell Tissue Bank 2015.
- Hermans MH. Preservation methods of allografts and their (lack of) influence on clinical results in partial thickness burns. Burns 2011;37(5):873-81.